Projecting the Future Supply of Pediatric Subspecialists in the United States 2020-2040
Overview
Concerns persist about whether the United States (US) has an adequate supply of pediatric subspecialists and whether they are appropriately distributed across the nation to meet the health care needs of children. This website presents a workforce projection model that estimates the future supply of pediatric subspecialists in clinical practice in the US from 2020-2040. The model's supply projections can be viewed in conjunction with other data to provide insight into the future of the pediatric subspecialty workforce and offer data to inform decision-making.
Methods
The model uses a microsimulation approach. The methods address important limitations of prior workforce projections that have grouped adult and pediatric physician subspecialty workforces together and aggregated pediatric subspecialties together into one projection. This website allows users to visualize and compare model forecasts of the future supply of 14 pediatric subspecialities at the national, census region and census division level. The model is also novel because it accounts for the geographic moves that pediatric subspecialists make after training and during their career.
The supply forecasts are based on historical data from the American Board of Pediatrics. Ten “what if” scenarios allow users to simulate the effect of changes in the number of fellows entering training, the rate at which subspecialists leave the workforce, and changes in hours worked in direct and indirect clinical care. The model provides estimates of both the future headcount (HC) of subspecialists and HC adjusted for self-reported proportion of time spent in clinical care, termed “clinical workforce equivalent” (CWE). CWE is a more robust measure of available clinical supply of pediatric subspecialists in the US because most pediatric subspecialists are affiliated with academic medical centers and spend time in medical education, administration, quality improvement, or research.
Key Findings
The projected growth of the pediatric subspecialty workforce does not align geographically with projected growth of the child population. The South and West census regions are projected to increase their child populations (0-18) faster than the Northeast and the Midwest regions by 2040. Yet the supply of pediatric subspecialists is projected to be highest in the Northeast (Figure 1), a region where a large number of fellowship positions are located. The Northeast census region is projected to see a 4% growth in the child population (0-18 years) compared to the South where the child population is forecast to grow by 19% growth and the West which is expected to increase by 23%.
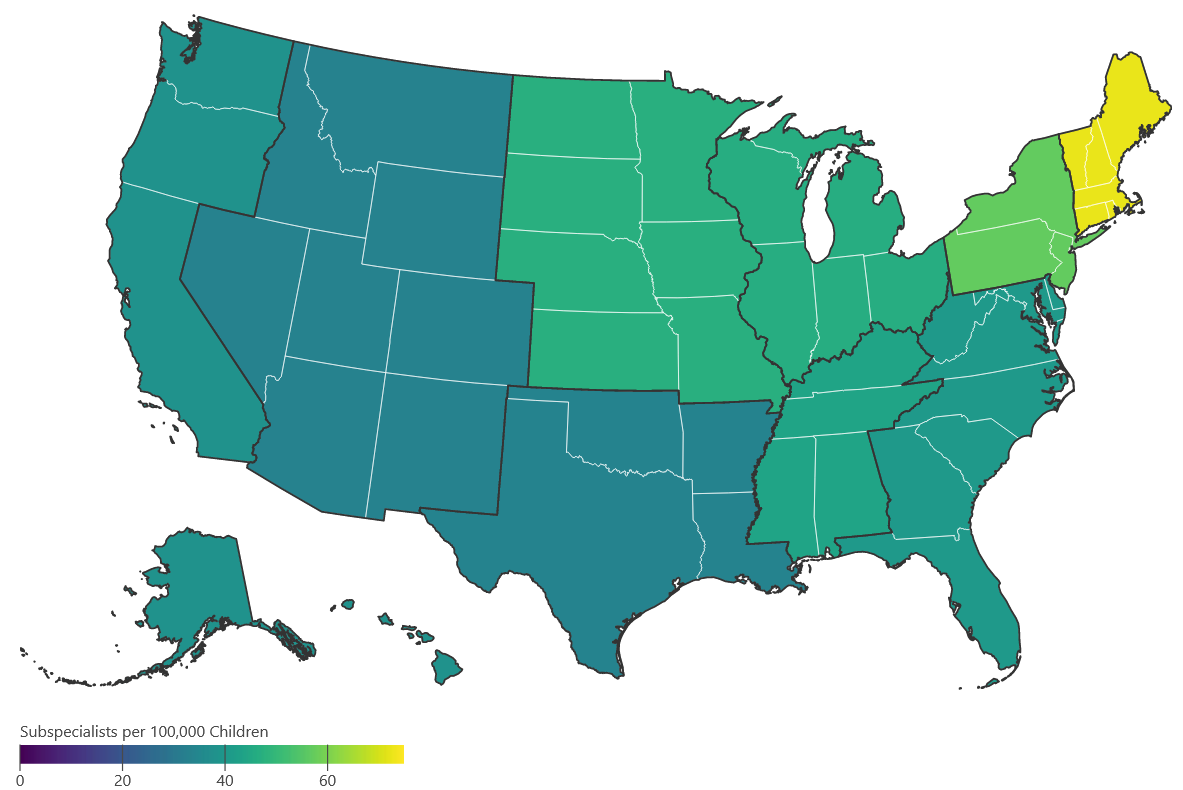
Implications: Some US census divisions and regions may face gaps in access to care if action is not taken to improve the geographic distribution of pediatric subspecialists. Since more than half of recently trained fellows end up in practice in the same census division where they trained, developing new fellowships, and expanding existing training programs in the South and West could help ameliorate shortfalls.
The Current Supply and Projected Growth Varies Significantly between Subspecialties. Subspecialties are vastly different in terms of the size of the workforce, measured by HC and CWEs. They also differ in terms of their projected growth.
Headcount: Of the 14 subspecialities, 9 had 1,000 physicians or more in the workforce as of 2000 whereas 3 subspecialities had fewer than 700 and 2 had fewer than 400. For example, there were 5,193 neonatal-perinatal medicine physicians in the workforce in 2020 or 6.38 per 100,000 children, compared to 653 adolescent medicine physicians or 0.8 per 100,000 children.
CWEs: After adjusting for self-reported hours in clinical care, the subspecialities ranged from 0.23 CWE to 4.36 CWE per 100,000 children in 2020. For example, there were 4.36 CWEs per 100,000 children in 2020 in neonatal-perinatal medicine compared .43 CWEs in adolescent medicine, meaning that the neonatal-perinatal medicine workforce providing clinical care is ten times the size of the clinical workforce in adolescent medicine.
Projected Growth: Projected growth of subspecialties between 2020-2040 ranges from 24% and 105% in headcount and 22% to 102% in CWE. For example, the headcount of the neonatal-perinatal medicine workforce is projected to increase by 42% in headcount and 41% in CWE between 2020 and 2040. By contrast, adolescent medicine will grow at a significantly lower rate, increasing by 27% in headcount and 28% in CWE.
Implications: Analyses of the pediatric subspecialty workforce that seek to understand future supply and adequacy of that supply need to consider each subspecialty individually. Subspecialties with a smaller HC and CWE in 2020 and those that are projected to grow more slowly (e.g., developmental-behavioral pediatrics, pediatric endocrinology) may struggle to meet future clinical care needs. Subspecialties that have larger HC and CWE and those that are forecast to grow more quickly (e.g., pediatric cardiology) may have a sufficient supply at the national level, if historical trends continue.
Ready to Start Exploring?
This website has an Interactive Model that lets you compare different projections and an Interactive Map.
Who Developed the Model?
The Principal Investigator of the model is Erin Fraher PhD MPP, Director of the Program on Health Workforce Research & Policy at The Cecil G. Sheps Center For Health Services Research at the University of North Carolina. The model was developed in partnership with Strategic Modelling Analysis & Planning Ltd and The American Board of Pediatrics Foundation, which funded the development of the model and this website.
Interested in More Findings?
A supplement issue of the journal Pediatrics was released in February 2024 that contains 19 articles, authored by more than 50 workforce experts from each of the pediatric subspecialties. These articles examine the current landscape for pediatric subspecialties, provide commentary on how to interpret the model findings, and present recommendations for education and training, practice, policy, and research.